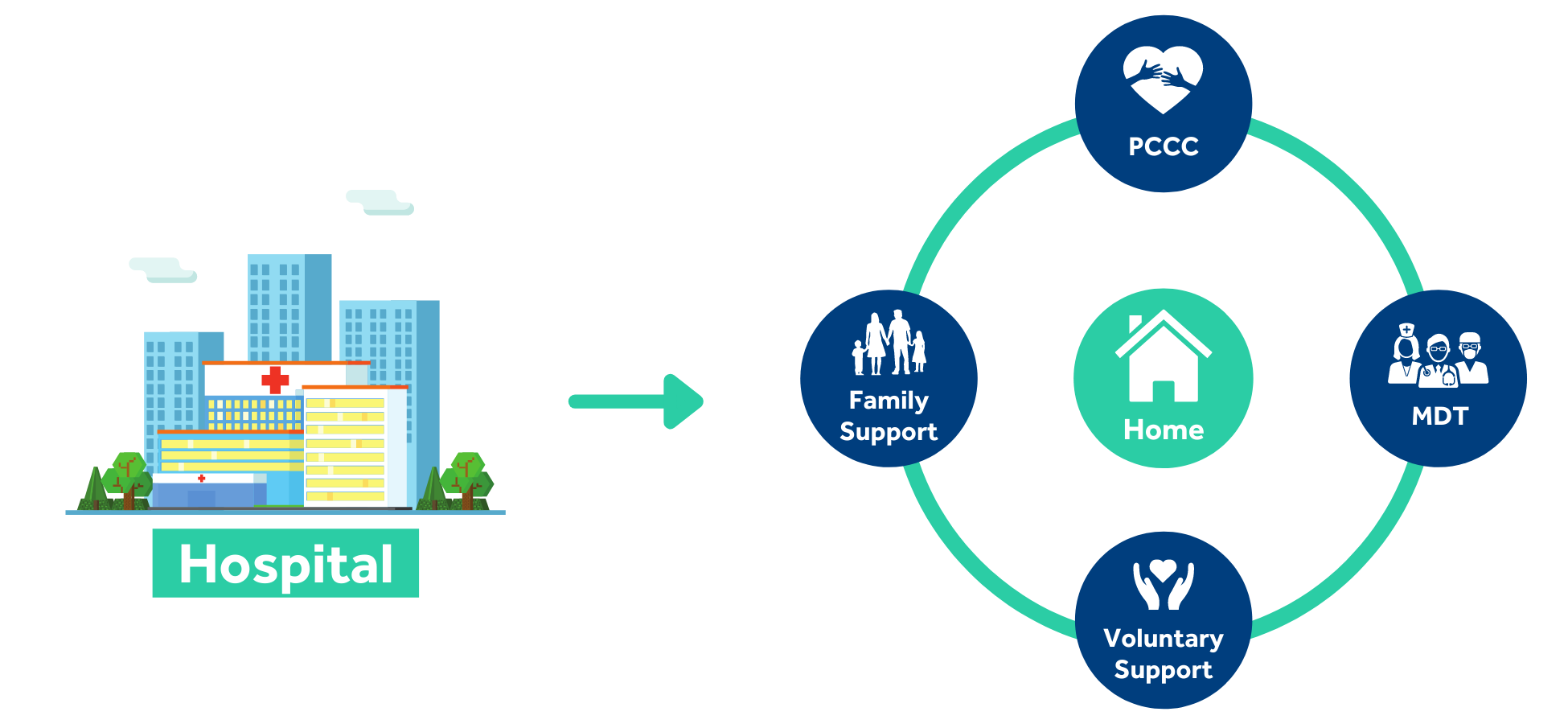
Seamless discharge from hospital to home
The concept of Rapid Response is to facilitate the timely discharge and smooth transition of service users from hospital to home, thus reducing the number of hospital admissions and allowing service users to remain independently at home for as long as possible. Our aim is to manage the needs of individuals from birth to retirement and beyond.
Rapid Response Team
Our rapid response team is on call 24 hours a day, 365 days a year and they are available to cater for the service user’s individual needs at any point in time, day or night.
From our initial point of contact right through to the implementation of therapeutic interventions, each service user is provided with a systematic, empathetic and consistent approach to enhancing their health and well- being and increasing their quality of life.
We believe we provide an invaluable service to our very valued and cherished service users.

Current Process
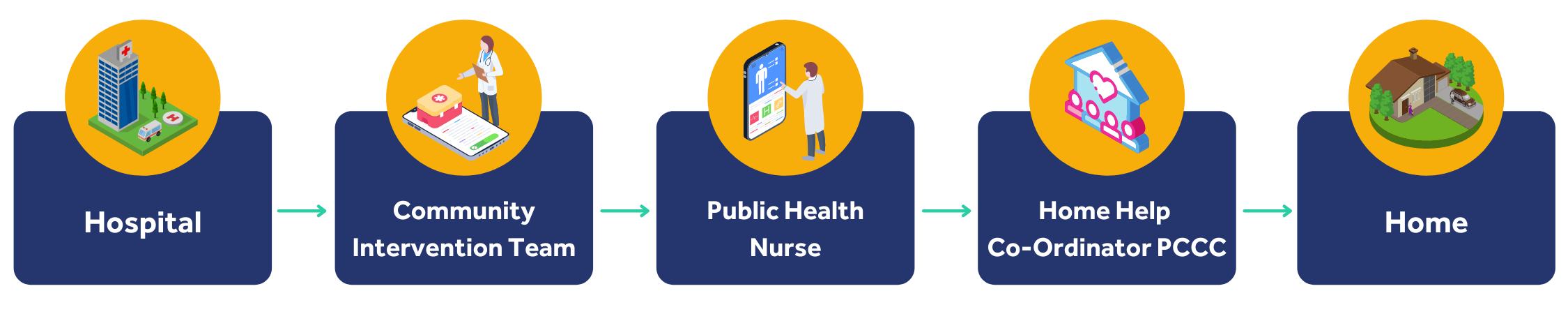
Rapid Response Process
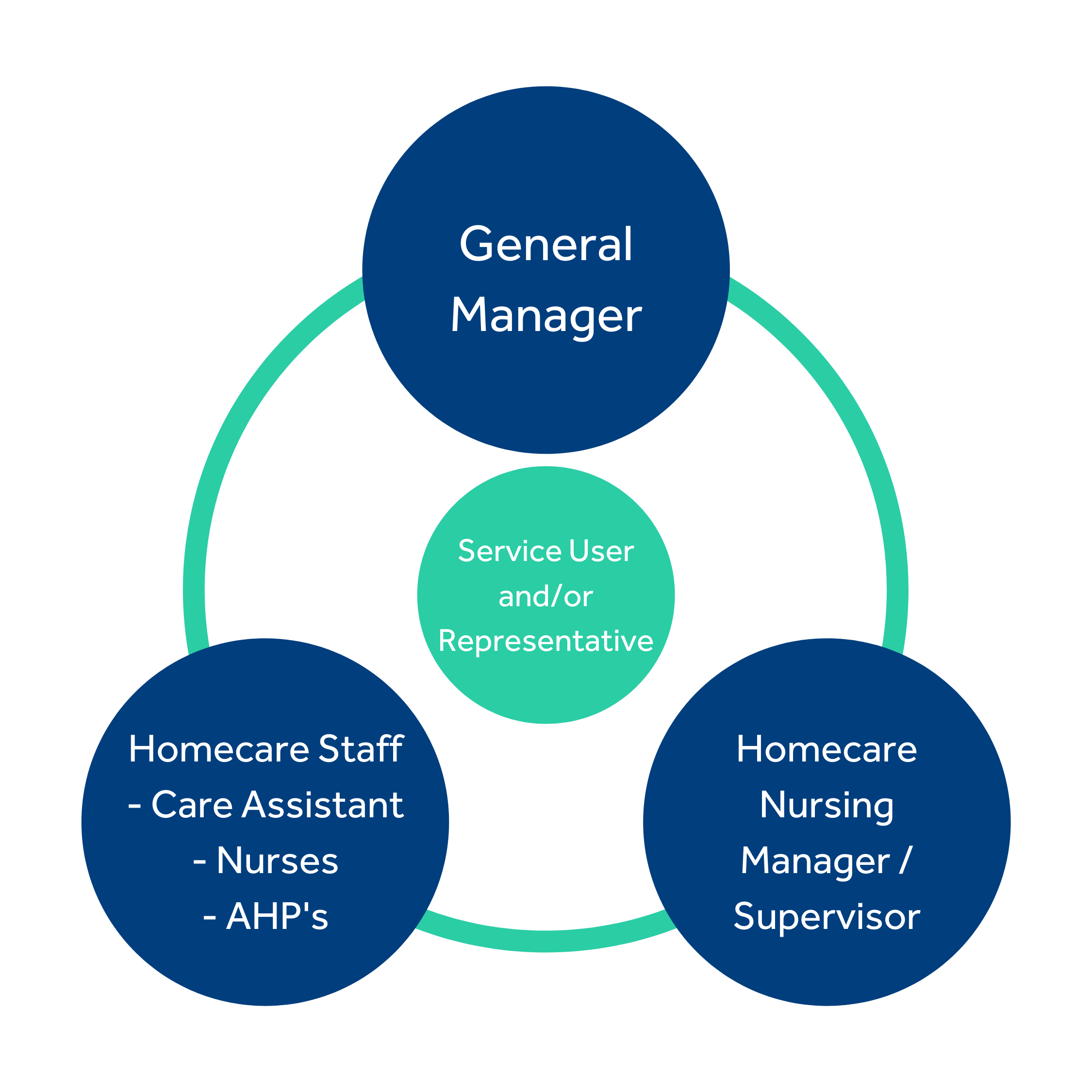
With all the supports already in place, the Myhomecare Nurse Manager co-ordinates the process from start to finish.
Standard of Service
This service uses a person centred delivery care system in order to meet each client’s individual core needs. We believe that each service user should receive the highest standard of care possible and we strive to deliver care that acts within the best interests of the client at all times in the most populated areas and the most remote areas. It has long been our mission statement to change, for the better, on a daily basis the way we deliver excellence and value to our service users in the provision of healthcare services. Maintaining respect, dignity and integrity are fundamental principles in the delivery of care. We encourage each service user to become actively involved in the assessment, planning, implementation and evaluation stages of the care process.
The success of this model has been based on the collaboration with all services and clinicians relevant to the service user, thereby providing a deeply holistic, individualised service. We offer much more than a homecare package, we have a number of value added services such as assisted living programmes, continued and palliative care programmes and advanced physical and mental health care programmes. But most importantly, it is our aim to deliver care that is tailored to meet the specific needs of the individual, focusing on choice, identity, hope, personal abilities, strengths and goal setting in order to achieve positive outcomes. We believe that the service user is central to the effective delivery of quality of care and it is of paramount importance for the client to feel safe, secure and supported within the comfort of their own home.
Case Studies
58 year old lady admitted due to sustained injury from a fall. Discharge delayed due to lack of family support at home.
Referral received from the hospital discharge liaison officer. Initial assessment and care plan carried out on-site with stakeholders, service user and homecare coordinator from Myhomecare. Transport and collection of medication arranged for discharge later that day.
Homecare staff required for close supervision of mobility, medication prompting, assistance with activities of daily living and monitoring of physical and emotional well-being. Input provided from physiotherapist.
Aims/Objectives: To reduce risk of readmission to hospital, to prevent injury/falls, to maintain a safe environment, to increase social support.
5 month old baby with tracheostomy and peg fed in-situ discharged home following recurrent infection.
Referral received from community intervention nurse. Initial assessment carried out with all stakeholders, service user and family. Care plan discussed and placed in service user’s home. Input provided from early intervention nurse.
Paediatric nurse required during the night to allow rest time for family, to monitor tracheostomy and peg feed, observe and check vital signs and to observe and report any signs of infection.
Aims/Objectives: To prevent infection, reduce the risk of possible admission to hospital, to maintain a safe environment and to ensure physical, psychological and emotional well-being.